Tomorrow’s Home: A Salutogenic Role in Health Management
Date
January 22, 2019In 2017, 18% of the UK population was over the age of 65 and 2% were over the age of 85. By 2050 nearly one in five people in developing countries will be over 60. The needs, challenges, and expectations of this group will be significantly different than those of previous generations.
At the same time, chronic and lifestyle-related diseases are on the rise, and healthcare services are struggling to keep up with the consequent accelerating demand. The recently published NHS Long Term Plan has called for the need for action on prevention and mainstream digitally-enabled care.
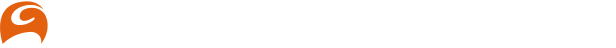
The focus must be toward delivering a ‘new look’ service that’s embedded within communities. This could range from assisted living, self-care, tele-care, and tele-medicine within a single housing unit, to multiple units supported by social care services, nurses, doctors, physiotherapists, occupational health visitors, psychiatric nurses, and local pharmacists.
Digital tools enable healthcare services to be more personal and socially-minded. Click here to view larger image.
Technology and communication networks can help alleviate overburdened healthcare systems by providing clinical tele-health and tele-care services to people on demand. Companies such as Amazon, Google, and Microsoft are already establishing their digital presence within our homes and it’s not hard to imagine this infrastructure enhanced by tele-healthcare services. With high definition video tele-healthcare systems, doctors and nurses will be able to hold virtual consultations with patients or remote in from hospitals in a “virtual ward” scenario. Already, there are successful examples of real-time clinical tele-health services such as tele-mental health, tele-audiology, and tele-nursing that use monitoring sensors to capture and transmit physiological data.
This shift will also see a rise in salutogenesis, an approach that focuses on factors that support human health and well-being not only within the community, but also in the homes of tomorrow.
In order to best design the home care services of tomorrow, the ageing process, body systems maturity, human physiology, and sensory receptors must be understood alongside the comprehension of related medical issues, morbidity levels, and salutogenic needs. However, in order to address the health and wellbeing issues of today and tomorrow, the traditional perceptions of what constitutes as “home” will have to be dismantled, reinvented, and reconstructed. These new spaces must be flexible and agile to adapt to ‘ageless’, ‘multigenerational’, and ‘multi-morbidity’ scenarios.
Ergonomic and anthropometric data can be used to help design a supportive home with fabrics, and finishes, equipment, and devices designed to accommodate the ageing body: its predicted postures, movements, weight, size, properties, and cognitive abilities. Design tools such as virtual reality, augmented reality, and sense-sensitive design will ensure successful outcomes.
Assistive design and technology interventions do not have be disruptive or expensive. Correcting diurnal temperatures, colour ways, bedside dimmers, bed inclination, amber illumination, bed/WC orientation, and biophilic design, are all examples of low-barrier interventions. Alternative solutions are available as well, though they tend to be more costly. Examples of these include, medical bedheads, sensory doors, body driers, robotics, thermal responsive shower heads and tiles, smart floors, LED WC seats, smart oxygen delivery, night-time hydrants, LED pillows, axo suits, Toto WC/Bidets, ODE emitters and Tomek fittings.
While there are many challenges facing healthcare systems, today’s rapid technological advances offer us a solution to provide new and innovative forms of healthcare services that can improve what’s currently available. If we embrace today’s challenges and deconstruct, reconstruct, and reboot them with a focus on health and well-being, the homes of the future could well alleviate the pressures that our current healthcare systems are struggling with.
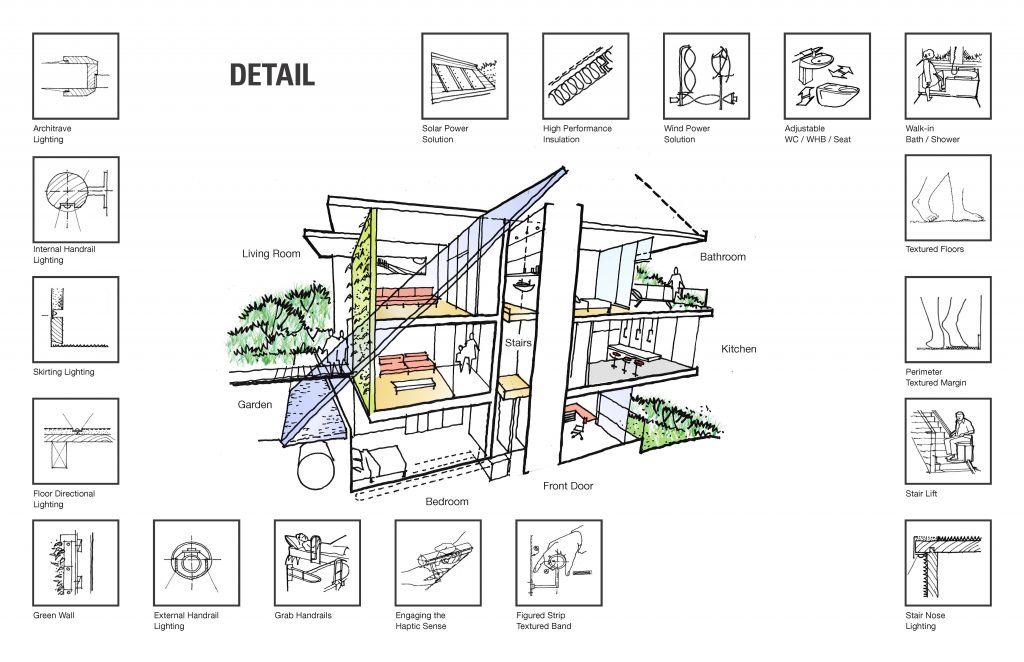
Ergonomic and anthropometric data can help the next generation of elders age in place. Click here to view larger image.
This article is based on the findings of the UK Government White Paper, Neighbourhoods of the Future, produced by the Agile Ageing Alliance in partnership with Tata Steel.
Photo by Philippe Leone on Unsplash
Richard Mazuch is an architect and designer who gains great satisfaction from translating holistic ideas into radical but pragmatic solutions. An authority on healthcare, Richard provides profound insight into designing for global trends, patient groups and clinical provision – informing key decisions throughout the architectural process. Richard has worked on healthcare projects in Italy, Hong Kong, Brazil, Oman, UAE, and more recently Australia. He has been elected as a World Architecture Jury member, as well as being a University lecturer/examiner and speaker at the International Conferences. Richard has strong relations with key health bodies. He has worked extensively with the NHS contributing to Health Building Notes, Health Technical Memorandum, and their ‘therapeutic environment’ website feature entitled “Slight Sensitive Design and Sound Sensitive Design” enabling designs to build evidence-based healthcare environments. Richard is a founder and champion of IBI TH!NK. An advocate of evidence-based design, Richard creates innovations that positively impact the psychology and physiology of patient groups. Sense Sensitive Design, Emotional Mapping, the Design Prescription and the hPod are a few of the models that Richard has successfully pioneered. This has led to him co-authoring two new NHS guidelines for ‘Evidence-based Design Healthcare Environments’. Richard works frequently with the NHS and DOH Expert Working Groups and Reference Groups helping to develop new Healthcare Strategies and Guidelines. More recently he has co-authored three key Paediatric Guideline documents entitled: ‘Hospital Accommodation for children and young peopleHBN 23’, ‘Friendly healthcare environments for children and young people’ and ‘Mental Health faculties for children and young people’. Richard was also an active member and contributor to the Expert Reference Group responsible for ‘Facilities for Maternity Care’ HBN21. He was a key contributor to ‘The Children’s National Service Framework’ an NHS and Department of Health document with evaluation process and recommendations Richard made early contributions and document reviews of ‘Creating a Better Health Environment’ an Audit Took Kit by The National Childbirth Trust in 2003.
Richard is a product designer. In collaboration with manufacturers, he creates interventions, such as the BedPod, to support and improve patient care.
In education, Richard is translating his work in healthcare paediatrics to benefit teachers and students. Working alongside University partners, he is pioneering the development of an ‘optimal learning environment’, improving motivation, behaviour and concentration amongst pupils, especially those with special educational needs.